The specialists at the Washington University Fertility and Reproductive Medicine Center have been helping families achieve pregnancy through in vitro fertilization (IVF) for over 30 years. In May 2005, families gathered at a reunion to celebrate their success through this program. One person present was the first baby born through the in vitro fertilization process.
IVF is an effective method for producing pregnancies. Today 1-2% of all births in the United States are a result of IVF.
IVF can seem overwhelming at first, but your doctor will explain the process carefully, setting expectations and a checklist of required steps.
There are a lot of myths and misunderstandings about what IVF is, what it costs, risks, what the success rates are, risks of multiples, etc. And everyone’s IVF experience can vary depending on their reason for doing IVF.
IVF is emotionally, physically, and financially taxing. Patients are encouraged to ask questions at any time. The more you know, the more relaxed the process can be.
What is IVF
In vitro fertilization (IVF) is a procedure in which eggs (oocytes) are retrieved from a the ovaries after the patient has undergone controlled ovarian hyperstimulation. The eggs are mixed (either conventionally or with ICSI) with the partner’s or donor’s sperm in a culture dish. Fertilization takes place without additional procedures.
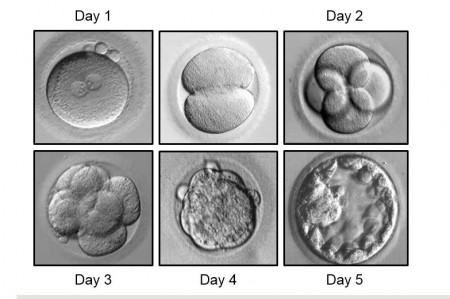
Most of the fertilized eggs should develop into embryos. The embryos are then transferred to the uterus via a plastic tube inserted through the cervix during a process called an embryo transfer. If all goes accordingly, the embryo(s) attach into the uterus in the normal way, and pregnancy progresses naturally. We encourage certain, eligible patients to consider the transfer of one embryo to reduce the risks of multiples.
As noted above, depending on each patient’s situation, many variations can occur during this process.
IVF is a multi-step process
- Prestimulation
- Physician plan – individualized to the family’s needs
- Medical and financial clearance
- Scheduling of the cycle
- Stimulation/Monitoring
- Baseline testing/monitoring and stimulation of the ovaries
- Egg retrieval
- Embryo transfer (Day 3 or Day 5 embryos)
- Pregnancy test
What are your success rates?
Please visit Society for Assisted Reproductive Technology (SART) for success rates concerning fertility clinics.
SART membership
Our center is a member of the Society for Assisted Reproductive Technology (SART). SART’s mission is to set and help maintain the standards for assisted reproductive technology (ART), in an effort to better serve both members and patients. SART governs its members in the areas of research, quality assurance and practice guidelines and standards, government interaction, and data collection. SART members adhere to the highest standards of reproductive care.